Quality Improvement Projects
All physicians share responsibility for promoting patient safety and quality improvement in health care. During training, programs must prepare residents to provide the highest level of clinical care with a distinct focus on patient safety, patient-centered care, and humanity of all.
Residents must demonstrate the ability to analyze the care they provide and play an active role in system improvement processes. It is necessary for residents and faculty members to work together within healthcare teams to achieve organizational patient safety goals.
- adapted from the ACGME Common Program Requirements
Our residency training program provides various opportunities for residents to play an active role in patient safety and quality improvement endeavors.
Hospital-based participation includes:
- Incident reporting for adverse events and near misses
- Participation in Root Cause Analysis
- Simulation training within the patient care environment (ex. ER Trauma Resuscitation Room or Labor & Delivery Suite)
- Participation in hospital committees, such as: Pharmacy & Therapeutics, Infection Prevention, OB Quality, OR Committee, etc.

Department-based participation includes:
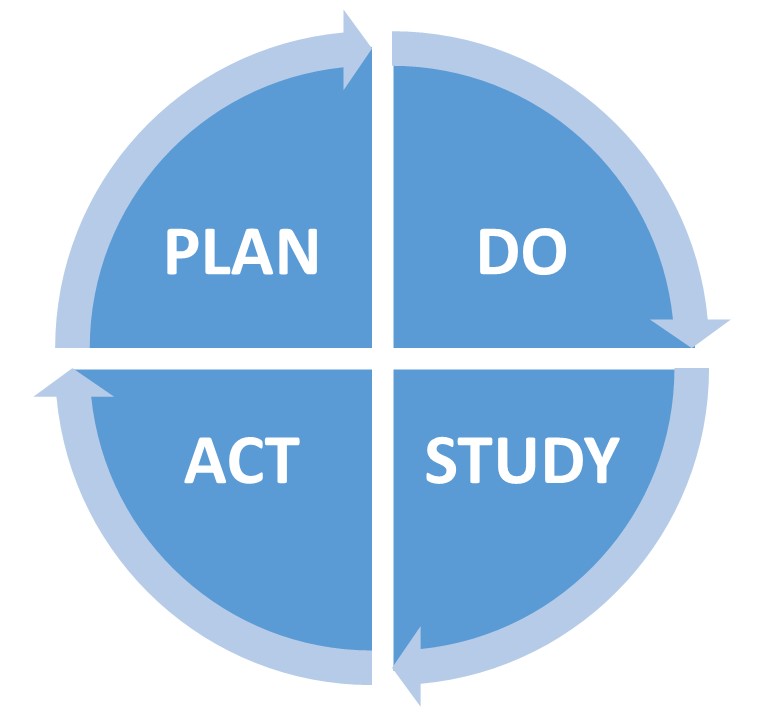
- education about quality improvement methodology
- review of clinical metrics: readmission rates, blood transfusions, C-section rates, and surgical site infections
- attendance at monthly patient safety conferences
- participation in a quality improvement project with a team of residents and a faculty mentor
The Department of OBGYN has been an active participant in the Annual QI/PS Forum for the LSU Health Sciences Center since its inception in 2013.
Recent or ongoing projects include:
- Implementation of a Protocol to improve Aspirin use in Pregnancy
- Optimization of a Remote Patient Monitoring Program for Hypertensive Disorders in Pregnancy
- Placenta Accreta Spectrum: A Needs Assessment for a Center of Excellence
- Reduction of Surgical Site Infection in Hysterectomy
- Timely use of Misoprostol on L&D in Postpartum Hemorrhage
- Univeral Substance Use Disorder Screening on L&D
